KFM and King's College Hospital NHS Foundation Trust Collaborate in Neonatal in-vitro Study
KFM and King’s College Hospital, recently collaborated in a neonatal in-vitro study aimed at researching the effect of inflation pressure on end-tidal carbon dioxide levels in neonatal care.
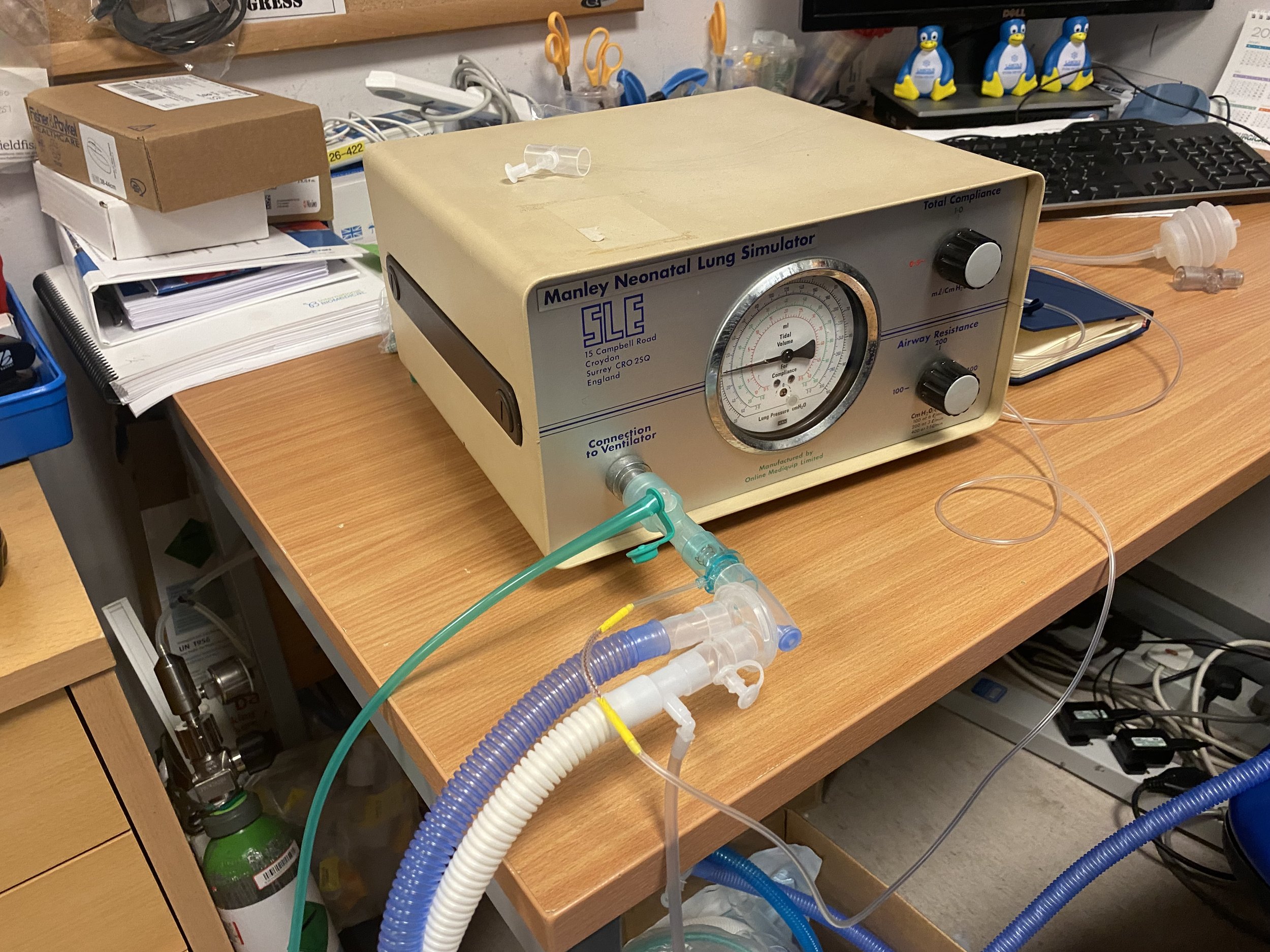
Jonathan Saka, KFM’s Lead Paediatric Technologist and co-author of the study, played a pivotal role in assembling a ventilator system. This system utilised a synthetic baby lung (test lung) to replicate the intricate complexities of a baby's lung. Three tests were carried out on different neonatal conditions;
Breathing trouble straight after birth (Respiratory Distress Syndrome/RDS)
Long-term lung disease (Bronchopulmonary Dysplasia/BPD)
A common cold in the lungs (Bronchiolitis)
Dr Theodore Dassios, Lead Researcher and Consultant Neonatologist at King's, said: “Jonathan is really brilliant in the Neonatal Unit, he is constantly there to support us when it comes to equipment needed for clinical purposes. He went out of his way to help me set up an in-vitro model for a neonatal study which mimicked a baby lung and which investigated the effect of altering the parameters of mechanical ventilation on the effect of exhaled carbon dioxide. His contribution was pivotal for the project.”
The results of the neonatal in-vitro study revealed that when the pressure increased, there was a corresponding decrease in carbon dioxide levels, and the most significant reduction in carbon dioxide was observed in the model representing Respiratory Distress Syndrome (RDS), indicative of severe breathing difficulties.
Understanding the link between pressure changes and carbon dioxide levels is crucial for designing improved ventilation systems, particularly for babies in hospitals. This research will be significantly beneficial to patients with conditions like RDS and BPD, help optimise oxygenation, minimise lung injury and improve outcomes for critically ill newborns.
Describing the effects of too much or too little carbon dioxide on neonates, Jonathan, Lead Paediatric Technologist, says: “Imagine your body is like a car. Cars need the right amount of gas to run well. For our bodies, the 'gas' is the air we breathe in and out. If a baby has too much carbon dioxide (which is like bad air) in their body, it's like putting the wrong fuel in the car. The car won't run well, and the baby might feel really tired or sick. On the other hand, if a baby doesn't have enough carbon dioxide, it's like not having enough gas in the car. The car might not start or run properly, and the baby might also feel unwell. Through this study, we've been able to understand how pressure changes affect carbon dioxide which will help design better machines for real babies in hospitals."
This remarkable collaborative project has the potential to significantly contribute to advancements in neonatal care, on a broader scale.